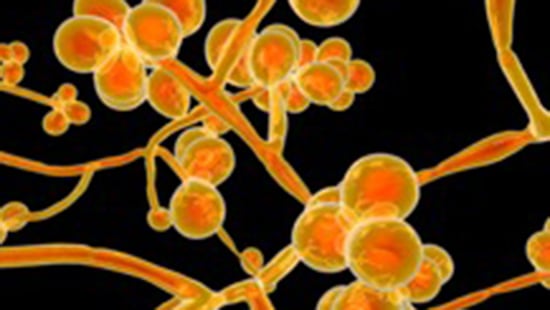
Candida Auris (c. auris)
What is Candida auris?
Candida auris is an emerging multidrug-resistant yeast that has caused severe infections in hospitalized patients and nursing home residents. C. auris can persist on surfaces and spreads easily between patients in healthcare facilities. C. auris may not be accurately identified using standard laboratory methods. For these reasons, proper infection control measures are important to prevent its spread. C. auris has been identified in over 30 countries worldwide including the United States and has been the cause of numerous outbreaks at healthcare facilities. C. auris has caused infections at numerous sites including surgical wounds and the inner ear. It has also been isolated from respiratory and urine specimens, although its ability to cause infections of the respiratory or urinary tract remains unclear. C. auris is also capable of causing serious, even fatal, bloodstream infections and invasive disease.
Infections have been found in patients of all ages, from preterm infants to the elderly. People who have recently spent time in nursing homes and those who have invasive medical devices such as breathing tubes, feeding tubes and central venous catheters seem to be at highest risk for C. auris infection. Other risk factors are similar to those observed for other types of Candida infection and include recent surgery, diabetes, and treatment with broad-spectrum antibiotics or antifungal agents. CDC recommends that anyone who believes they may have a fungal or healthcare-associated infection contact their healthcare provider.
WHAT ARE THE SYMPTOMS?
Symptoms of C. auris infection are often dependent on the location of the infection. C. auris has been implicated as the cause of bloodstream infections, wound infections, and ear infections. For severe or invasive C. auris infections, fever and chills are common. Many C. auris infections are treatable, however, some C. auris infections have demonstrated resistance to the three main classes of antifungal drugs currently in clinical use. Infections caused by highly drug-resistant strains of C. auris are much more difficult to treat.
C. auris has caused severe invasive infections, particularly in very ill patients in hospitals and nursing homes with underlying medical conditions. Severe infection caused by any Candida species can be fatal and more than 1 in 3 patients with invasive C. auris infection die2. and it is not known if invasive C. auris infection has a higher mortality rate than invasive infection caused by other Candida species. Based on information from a limited number of patients, 30–60% of people with C. auris infections have died.
HOW IS IT TRANSMITTED?
C. auris can spread in healthcare settings through contact with contaminated environmental surfaces or equipment where it can persist for several weeks. It can also spread directly from person to person.
HOW IS IT CONTROLLED?
The most important infection control measures for C. auris in acute care hospitals and high acuity post-acute care settings are as follows:
- Place the patient with C. auris in a single-patient room and use Standard and Contact Precautions
- Emphasize adherence to hand hygiene
Reinforce the importance of hand hygiene on the unit where a patient with C. auris resides. Use alcohol-based hand sanitizer or, if hands are visibly soiled, wash with soap and water. Wearing gloves is not a substitute for hand hygiene. - Clean and disinfect the patient care environment and reusable equipment (daily and terminal cleaning) with recommended products
C. auris can persist on surfaces in healthcare environments for weeks. C. auris has been recovered from many locations within patient rooms. This includes high touch surfaces such as bedside tables and bedrails as well as locations further away from the patient like windowsills. C. auris has also been found on mobile equipment including glucometers, thermometers, blood pressure cuffs, ultrasound machines, nursing carts, and crash carts. Meticulous cleaning and disinfection of both patient rooms and mobile equipment is necessary to reduce the risk of transmission.
Quaternary ammonium compounds (QACs) are routinely used in healthcare settings for disinfecting surfaces and equipment but may not be effective against C. auris. The CDC recommends using an EPA-registered hospital grade disinfectant that is effective against C. auris (EPA’s List P). If these products are not accessible, facilities may use products effective against Clostridioides difficile spores (EPA’s List K).
It is important to follow manufacturers’ directions for use of the surface disinfectant, including applying the product for the correct contact time.
Data on hands-free disinfection methods, like germicidal UV irradiation, are limited, and these methods may require cycle times similar to those used to inactivate bacterial spores (e.g., Clostridioides difficile) when used for C. auris.
- Ensure information about the patient’s C. auris and isolation status is fully communicated when they transfer to another healthcare facility.
- Screen patients who are at high risk for C. auris colonization, such as:
- Epidemiological link to a known case of C. auris
- Risk factors for acquiring C. auris, such as healthcare exposure in a part of the United States with a high burden of C. auris, international healthcare exposure or encounter in facility with suspected or confirmed transmission.
- See CDC website for more information on screening strategies based on different scenarios.
- Conduct surveillance for new cases to detect ongoing transmission.
References
Last update: March 2024
- www.cdc.gov/drugresistance/pdf/threats-report/candida-auris-508.pdf
- www.cdc.gov/fungal/candida-auris/candida-auris-qanda.html
- www.cdc.gov/fungal/candida-auris/tracking-c-auris.html
- www.epa.gov/pesticide-registration/list-p-antimicrobial-products-registered-epa-claims-against-candida-auris
- Cadnum, J., Shaikh, A., Piedrahita, C., Jencson, A., Larkin, E., Ghannoum, M., & Donskey, C. (2018). Relative Resistance of the Emerging Fungal Pathogen Candida auris and Other Candida Species to Killing by Ultraviolet Light. Infection Control & Hospital Epidemiology, 39(1), 94-96. doi:10.1017/ice.2017.23
_


