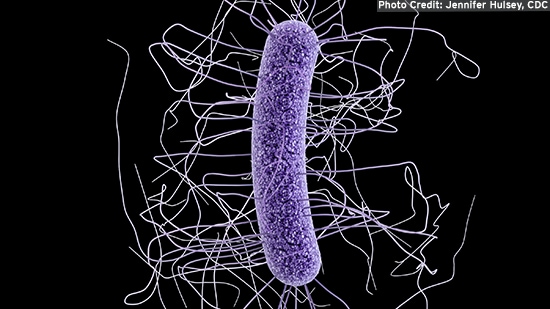
Clostridioides difficile
WHAT IS CLOSTRIDIOIDES DIFFICILE (C. DIFFICILE)?
Clostridioides difficile (C. difficile), formerly Clostridium difficile, is a bacterium that causes diarrhea and more serious intestinal conditions such as colitis. It is the most frequently identified cause of hospital-acquired diarrheal infection. The United States Center for Disease Control and Prevention (CDC) in collaboration with state health departments estimate that C. difficile causes almost half a million illnesses each year in the U.S. resulting in 29,300 deaths. About one quarter of these illnesses occurred in hospital settings. Nursing homes and outpatient healthcare settings were also cited as significant sources of C. difficile infection1.
C. difficile forms an endospore or a dormant state with increased resistance when conditions in the human or animal body or the environment become unfavorable for it to survive in its vegetative (actively growing) state. In the endospore stage, C. difficile spores will not be destroyed on environmental surfaces by disinfectants. The combination of the presence of C. difficile in hospitals and healthcare settings and the number of people receiving antibiotics in these settings can lead to frequent outbreaks.
WHAT ARE THE SYMPTOMS?
Healthy people usually are not susceptible to C. difficile disease. Patients requiring prolonged use of antibiotics and the elderly are at greater risk of acquiring this disease, and can be affected even by low numbers of C. difficile. Disease primarily occurs when the normal intestinal flora is altered, allowing the organism to flourish in the intestinal tract, attach to its walls and produce a toxin that causes a watery diarrhea. Researchers believe that antibiotic treatment is the greatest risk factor for patients, especially when clindamycin, cephalosporins, and penicillins are used – though virtually every antibiotic has been implicated. Advanced age, repeated enemas, prolonged nasogastric tube insertion and gastrointestinal tract surgery also increase the risk of infection.2
Symptoms include watery diarrhea, usually at a frequency of at least three bowel movements per day for two or more days, fever, loss of appetite, nausea and abdominal pain and tenderness. This can progress to colitis, sepsis and death in susceptible patients.3 People can continue to shed spores or cells after resolution of diarrhea. Since the bacteria are found in feces, people can become infected if they touch items or surfaces that are contaminated with feces and then touch their mouth or mucous membranes. If ingested, C. difficile spores generally resist the acidity in the stomach and can germinate in the small intestine.
HOW IS IT TRANSMITTED?
Hands of personnel, as well as a variety of environmental sites within institutions, have been found to be contaminated with C. difficile, which can persist in spore form.4 Asymptomatic people who are colonized with C. difficile can be a source of transmission of the disease to others. It can be part of the normal intestinal flora in as many as 50 percent of children under age 2, and much less frequently in individuals over age 2. The colonization rate in healthy adults is about 3 percent, but this increases to nearly 20 percent in elderly adults housed in chronic care wards.5
C. difficile may also occur ubiquitously in the environment in the spore form, surviving for five months on hard surfaces.6 The vegetative or spore form of C. difficile can be transmitted from contaminated surfaces by patients and/or healthcare workers and caregivers via the fecal/oral route. The primary route is from a patient with an active infection to others via healthcare workers hands.
HOW IS IT CONTROLLED?
Evidence for contamination of the hospital environment by C. difficile is compelling and aggressive cleaning and disinfection is effective in reducing the number of C. difficile positive cultures in the environment. Per EPA regulations, disinfectant products need to have sporicidal claims. In fact, the US EPA has required the removal of C. difficile vegetative claims from all EPA registered product labels.
Stringent hand washing practices are absolutely essential for minimizing the transmission of the disease via the hands. Proper hand hygiene can interrupt the potential disease transmission from person to person. While alcohol-based hand hygiene products are effective in promoting hand hygiene compliance, most are not effective against the spores of C. difficile. In the case of a C. difficile outbreak, traditional hand washing with soap and water for the mechanical removal and rinsing of spores from the hands is recommended.
CDC has published guidelines for isolation precautions in health care facilities.7 Considerations include placing patients in private rooms, using appropriate personal protective equipment, limiting patient transport outside their room, and implementing appropriate cleaning and disinfecting procedures.
REFERENCES AND FURTHER INFORMATION
1Lessa et al, 2015. Burden of Clostridium difficile infection in the United States. N Engl J Med. 372: 825-834.
2Samore, M.H. 1999. Epidemiology of Nosocomial Clostridium difficile diarrhoea. J Hosp Infect. 43 Suppl:S183-90.https://www.ncbi.nlm.nih.gov/pubmed/10658778?dopt=Abstract
3Clostridioides Difficile Infection | CDC - https://www.cdc.gov/HAI/organisms/cdiff/Cdiff_infect.html
4Gerding DN, Johnson S, Peterson LR, Mulligan ME, Siolva J Jr. 1995. Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol. 16:459-477.
5Rudensky, B., at al. 1993. The prevalence and nosocomial acquisition of Clostridium difficile in elderly hospitalized patients. Post-grad Med J. 60:45-47.
6Kim, K.H., et.al. 1981. Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic associated colitis. J. Infect. Dis. 143(1):42-50.
7CDC Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 -https://www.cdc.gov/infectioncontrol/guidelines/disinfection/index.html


